QPP/MIPS Educational Resources
I. Medicare Payment Overview
The Medicare Access and CHIP Reauthorization Act (MACRA) was signed into law April 2015, repealing the flawed sustainable growth rate (SGR) and establishing a two-track Medicare physician payment system that emphasizes the transition to value-based payment and delivery. To implement MACRA, the Centers for Medicare and Medicaid Services (CMS) established the Quality Payment Program (QPP), whereby eligible clinicians will either participate in the Merit-based Incentive Payment System (MIPS) or join an Advanced Alternative Payment Model (APM).
With few APM options available for Mohs surgeons, the American College of Mohs Surgery (ACMS) created MohsAIQ, a CMS-recognized Qualified Clinical Data Registry (QCDR) that allows Mohs surgeons to participate in the MIPS track of QPP by reporting quality measures relevant to their practice.
II. What is Merit-based Incentive Payment System (MIPS)?
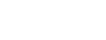
Performance Categories, Weights and Thresholds
MIPS incorporates four weighted performance categories – Quality, Cost, Promoting Interoperability, and Improvement Activities – that contribute to an annual MIPS final score of between 0 and 100 points. For 2023, if you score 75 points, you will avoid the 9% penalty. A score of 75.01-100 points qualifies you for a positive payment adjustment in 2025.
MIPS EUC Exception
CMS is continuing to allow MIPS EUC Exceptions for 2023. MIPS eligible physicians and groups may submit an application to reweight any or all MIPS performance categories if they've been affected by extreme and uncontrollable circumstances that impact these performance categories. This exception is not automatic - you must apply for reweighting of one or more MIPS performance categories. The application for the 2023 performance year will open in spring 2023 and will close at 8 p.m. ET on January 2, 2024. Additional information can be found on the QPP website.
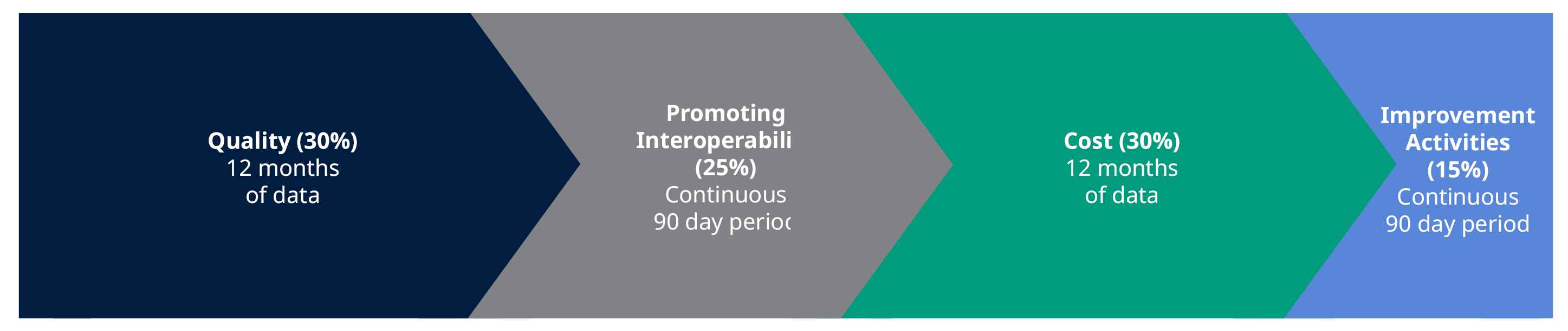
MIPS Eligibility
Are you eligible to participate in MIPS? Check here: https://qpp.cms.gov/participation-lookup
III. MIPS Participation
Brief Overview on Eligibility
Clinicians may participate in MIPS as individuals or as a member of a group (or virtual group). Individual clinicians (i.e., a single NPI tied to a single TIN) will have their payments adjusted based only on their performance. Clinicians that report as part of a group (i.e., identified by their NPI, who share a common TIN) will have their payments adjusted based on the group’s performance across all four MIPS categories.
Clinicians may also participate as a “virtual group,” which is a combination of two or more TINs made up of solo practitioners and groups of 10 or fewer eligible clinicians who come together virtually (regardless of specialty or location) to participate in MIPS for a performance period of a year. Learn more about this option by reviewing CMS’ Virtual Groups Toolkit.
Reporting Mechanisms
Clinicians may also choose to collect quality data via multiple mechanisms, including claims (limited to physicians in small practices), registry (i.e. MohsAIQ), certified electronic health record (CEHRT), and web-based attestation (via the QPP Portal). Clinicians may use different mechanisms across performance categories (e.g., report quality measures via claims and improvement activities via registry) and within performance categories (e.g., report quality measure A through claims and quality measure B through a registry).
VI. Alternative Payment Models (APMs)
Congress passed MACRA to incentivize participation in Alternative Payment Models (APMs). MACRA also created a second payment pathway, MIPS, for those not in APMs. MIPS was intended to be an on-ramp to APM participation.
An APM is a new payment approach to paying for medical care:
- Most often APMs utilize reimbursement methods that are different from traditional fee-for-service payments. However, APMs may retain fee-for-service payment elements as part of reimbursement structure.
- APMs require healthcare organizations (often hospital and affiliated physician practices) to align themselves with the goal of taking better care of a population of patients.
- Focus is on delivering higher quality of care rather than on the amount of care being given.
- APMs hold providers accountable for achieving specific quality performance goals in an efficient manner.
- Group practices participating in an APM receive added incentive payments to achieve the stated goals.
A common example of an APM is a Medicare Shared Savings Plan (MSSP), a.k.a. Accountable Care Organization (ACO). Under MSSP, if organization can realize savings by providing high-quality, low-cost care to a defined group of Medicare beneficiaries seen by the MSSP providers, Medicare will share savings with the ACO.
“Advanced APMs” are a subset of APMs that qualify for MACRA’s second payment track:
- Offers physicians and group practices incentives to provide high-quality, cost effective care under payment models that move away from fee-for-service payment system
- Providers must be in a qualifying Advanced APM and become a qualifying participant (QP) by achieving threshold levels of payments of patients
- Requires participants to use certified EHR technology
- Base payment on quality measures comparable to those in MIPS quality performance category
- Often require APM entities to bear more than nominal financial risk for monetary losses related to patient outcomes
- Advanced APM incentives:
- QPs receive an annual 5% lump-sum payment bonus, based on previous year’s Medicare part B payments. Bonus applies in payment years 2019-2024
- QPs are exempted from MIPS participation and payment adjustments
- Model-specific awards can also be designed within an APM framework